Vancomycin Toxicity Risk Calculator
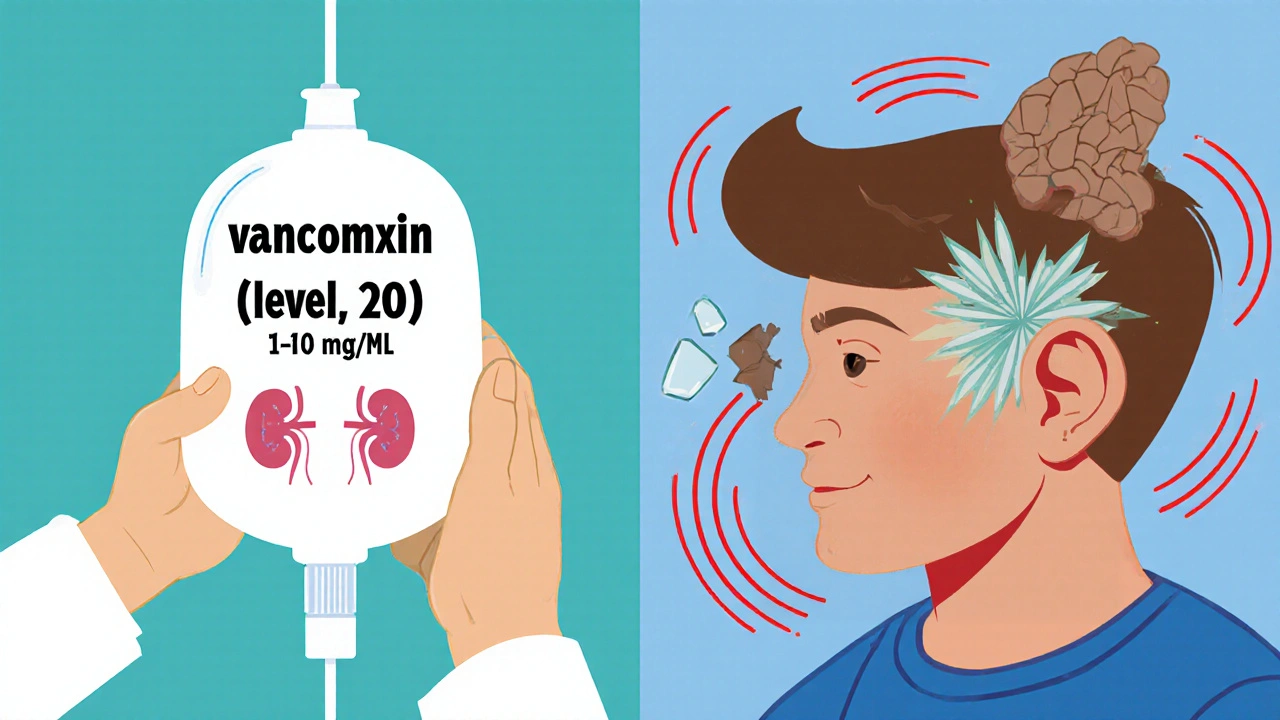
Nephrotoxicity Risk
Ototoxicity Risk
Vancomycin saves lives. It’s the go-to antibiotic for deadly infections like MRSA when nothing else works. But every time it’s given, doctors face a quiet, dangerous trade-off: protect the patient from a life-threatening infection, or risk permanently damaging their hearing or kidneys. This isn’t theoretical. Every year, hundreds of hospitalized patients in the U.S. and Europe develop kidney injury or hearing loss directly linked to vancomycin. And the worst part? Many of these cases are preventable.
Why Vancomycin Still Matters
Vancomycin isn’t new. It’s been around since the 1950s, but it hasn’t been replaced-not because it’s outdated, but because it still works when other drugs fail. For severe Gram-positive infections, especially those caused by drug-resistant bacteria, vancomycin remains one of the few reliable options. It’s used in ICUs, post-surgery wards, and for patients with compromised immune systems. But its power comes with a price tag written in biological terms: kidney damage and hearing loss.
Modern vancomycin is purer than the old versions from the 1970s, which had impurities that caused kidney damage in over half of patients. Today’s formulations are cleaner, but the risk hasn’t disappeared. In fact, new combinations with other antibiotics have made the problem worse.
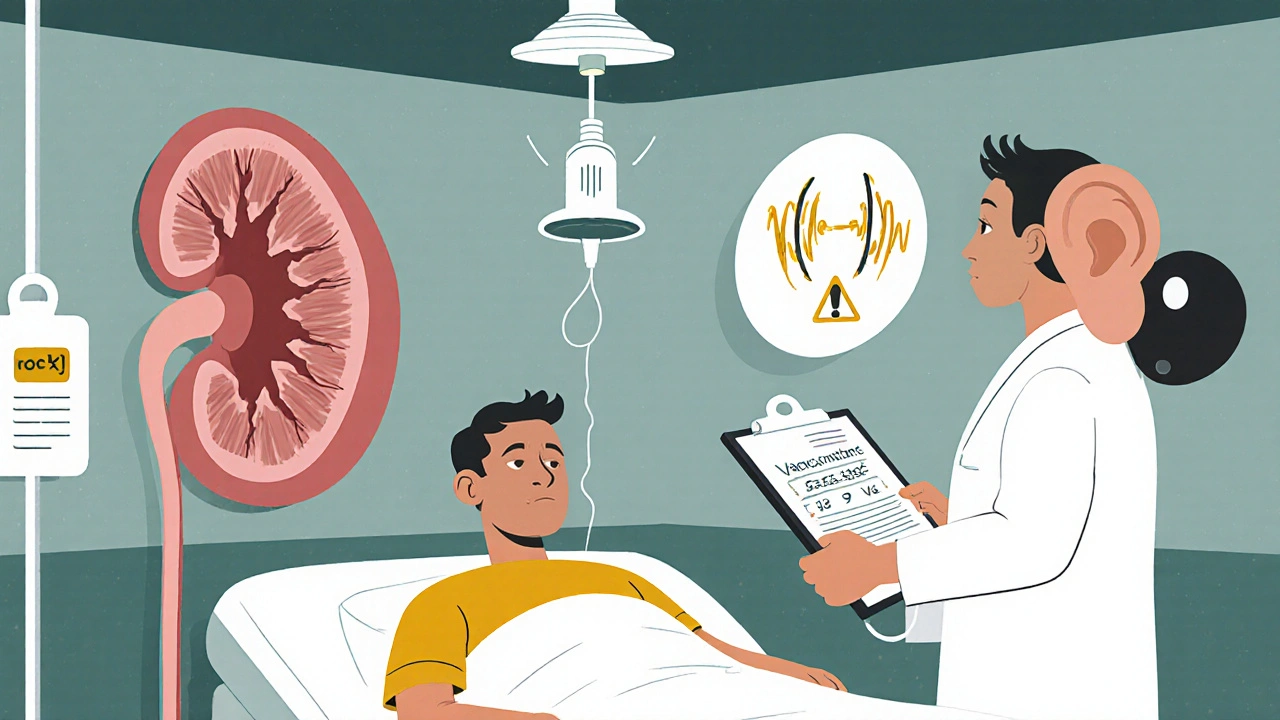
Nephrotoxicity: The More Common Threat
Nephrotoxicity-kidney damage-is the most frequent side effect. Between 5% and 30% of patients on vancomycin develop acute kidney injury (AKI), depending on their health, dosage, and what else they’re taking. The risk spikes dramatically when vancomycin is paired with piperacillin-tazobactam. A 2022 analysis of over 14,500 patients showed that this combo increased AKI risk by more than double compared to vancomycin with meropenem.
Why does this happen? Vancomycin directly harms the kidney’s tubules, the tiny structures that filter waste. It triggers oxidative stress and disrupts energy production in these cells. The damage usually shows up between day 3 and day 14 of treatment. Signs include rising creatinine levels, reduced urine output, and fluid retention.
High trough levels (the lowest concentration of drug in the blood before the next dose) are a major driver. For years, doctors aimed for troughs of 15-20 mcg/mL to ensure effectiveness. But research since 2020 shows that levels above 15 mcg/mL sharply increase kidney risk without improving outcomes. The current standard? Keep troughs between 10-15 mcg/mL for most infections. That simple shift has already cut nephrotoxicity rates in hospitals that adopted it.
Other risk factors pile up: older age, pre-existing kidney disease, dehydration, sepsis, and long treatment courses (over 7 days). Doses above 4 grams per day also raise the odds. And it’s not just vancomycin alone-combining it with other nephrotoxic drugs like aminoglycosides or NSAIDs multiplies the danger.
Ototoxicity: The Silent, Irreversible Risk
While less common, ototoxicity-ear damage-is far more devastating. It affects 1-3% of patients, but unlike kidney damage, it’s often permanent. Patients lose high-frequency hearing first, then may develop ringing in the ears (tinnitus). In severe cases, they lose the ability to understand speech, even with hearing aids.
What’s scary is that ototoxicity doesn’t always follow the rules. You might expect it to happen only with very high drug levels or in patients with poor kidney function. But that’s not true. A 1981 case report documented hearing loss in a patient with perfectly normal kidneys. A 2023 case showed irreversible damage after just three doses. One patient in a 2017 study developed hearing loss even with trough levels under 20 mcg/mL-no warning, no obvious cause.
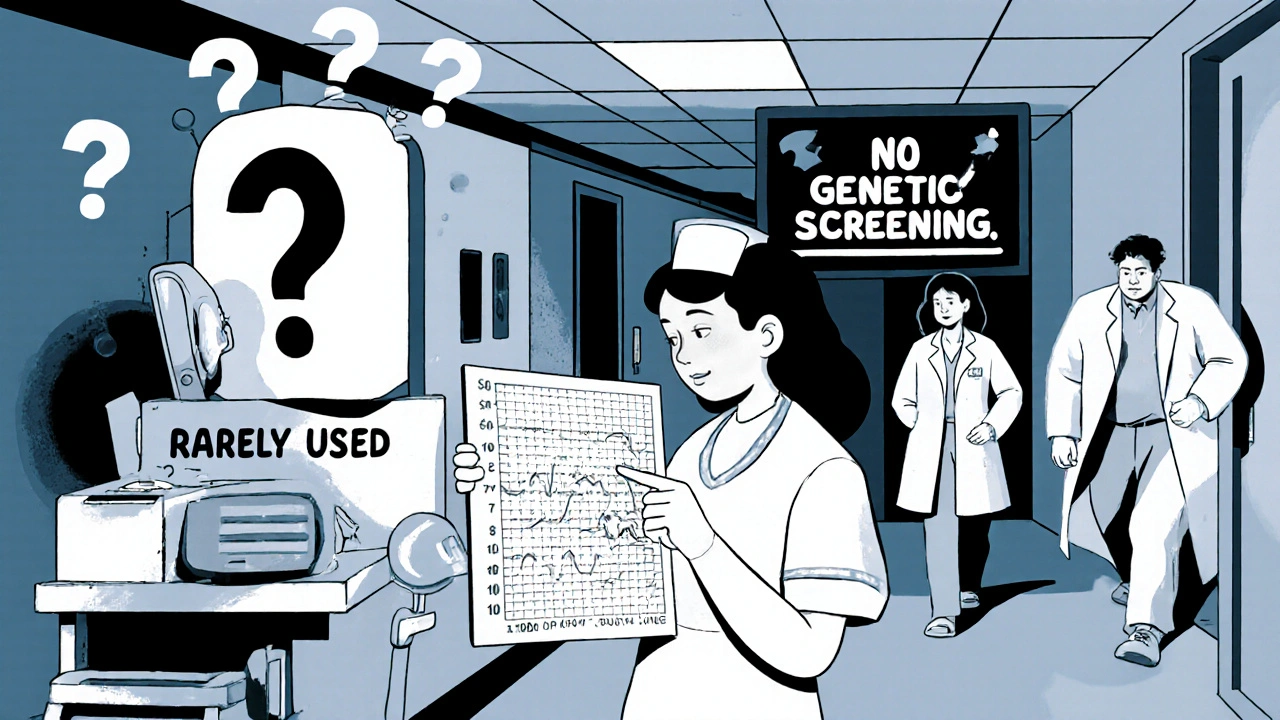
There’s no blood test for early ototoxicity. No lab value tells you it’s coming. Audiograms are the only reliable tool, but they’re rarely used. Only 37% of U.S. hospitals have formal protocols to screen for hearing loss in vancomycin patients. Many clinicians assume it’s rare enough to ignore. But when it happens, the impact is lifelong.
Peak drug levels, not just troughs, seem to matter more for ototoxicity. Concentrations above 80 mcg/mL are linked to irreversible damage. But even lower levels can hurt those with genetic susceptibility. A 2022 study found that people with a specific mutation in the MT-RNR1 gene are over three times more likely to suffer hearing loss from vancomycin. That’s a hidden risk no one tests for-yet.
Monitoring: What Works and What Doesn’t
For nephrotoxicity, monitoring is standard. Most hospitals check serum creatinine every 48-72 hours. Some use real-time pharmacokinetic tools like PrecisePK or DoseMeRx to calculate the area under the curve (AUC)-a better predictor of toxicity than trough levels alone. Hospitals using AUC-guided dosing see nephrotoxicity rates drop from nearly 15% to under 9%.
But for ototoxicity? The system is broken. Baseline and weekly audiograms are recommended for high-risk patients-those on high doses, long courses, or with prior hearing loss. But in practice, compliance is under 50%. Why? Audiologists are scarce. Tests are expensive. Staff are stretched thin. A 2022 cost analysis found routine audiometry only makes financial sense for patients with multiple risk factors. So most hospitals skip it entirely.
Some institutions are trying electronic alerts. One hospital cut vancomycin-piperacillin combinations by 22% after their EHR flagged the combo as high-risk. But no similar system exists for ototoxicity. There’s no algorithm predicting hearing loss. No flag for genetic risk. No quick test. That’s a gap in care.
When to Choose Alternatives
Vancomycin isn’t the only option. Daptomycin, linezolid, ceftaroline, and telavancin are alternatives-but each has its own problems. Daptomycin can cause muscle damage. Linezolid can wreck bone marrow. Ceftaroline is expensive and not always available. Telavancin still carries kidney risk.
So when should you avoid vancomycin? If a patient has pre-existing kidney disease, is elderly, or is already on another nephrotoxic drug, consider switching early. If they have a history of hearing loss, tinnitus, or are on other ototoxic drugs like furosemide or cisplatin, vancomycin should be a last resort. Genetic testing isn’t routine yet, but if a patient’s family has unexplained hearing loss, that’s a red flag.
For MRSA pneumonia or endocarditis, vancomycin is still first-line. But for skin infections or less severe cases, alternatives might be safer. The Infectious Diseases Society of America says vancomycin’s benefits usually outweigh risks-but only if you’re actively managing them.
The Bottom Line: Vigilance Over Assumptions
Vancomycin is a lifeline. But it’s also a landmine. We can’t stop using it. But we can stop pretending its risks are under control.
For nephrotoxicity: Keep troughs at 10-15 mcg/mL. Avoid piperacillin-tazobactam unless absolutely necessary. Monitor creatinine every 2-3 days. Use AUC monitoring if you can.
For ototoxicity: Assume it could happen-even with normal kidney function. Ask about hearing history. If treatment lasts more than 7 days or exceeds 4 grams daily, push for an audiogram. Document baseline hearing. If a patient reports ringing in the ears, don’t brush it off. Stop vancomycin and refer them.
There’s no perfect solution. But the data is clear: better monitoring saves kidneys. Better awareness saves hearing. The tools exist. The guidelines are there. What’s missing is consistent action.
What’s Next?
Research is moving fast. The 2023 VAN-GUARD trial showed real-time AUC dosing cuts kidney injury in half. Pharmacogenomics may soon let us screen for high-risk patients before giving the first dose. Point-of-care hearing tests are being developed. New vancomycin analogs with lower toxicity are in trials.
But until those arrive, the job falls to clinicians: watch closely, question combinations, listen to patients, and don’t assume safety because the drug is old. Vancomycin’s risks aren’t relics of the past-they’re active threats in today’s hospitals. Balancing them isn’t optional. It’s the standard of care.
Can vancomycin cause permanent hearing loss even with normal kidney function?
Yes. While vancomycin-induced hearing loss was once thought to occur only in patients with kidney problems, case reports since the 1980s have confirmed it can happen even with normal renal function. A 2023 report documented irreversible hearing damage after just three doses in a patient with healthy kidneys. Genetic factors, peak drug levels, and individual sensitivity appear to play key roles, making it unpredictable based on kidney function alone.
What vancomycin trough level increases the risk of kidney damage?
Trough levels above 15 mcg/mL significantly raise the risk of acute kidney injury. Studies show the nephrotoxicity risk curve steepens sharply past this point, with no added benefit for most infections. Current guidelines recommend maintaining troughs between 10-15 mcg/mL for most cases, and even lower (10-12 mcg/mL) for less severe infections to minimize harm.
Is vancomycin more toxic when combined with piperacillin-tazobactam?
Yes. Vancomycin combined with piperacillin-tazobactam increases the risk of acute kidney injury by more than double compared to vancomycin with meropenem. A 2022 meta-analysis of over 14,500 patients found this combination carries an odds ratio of 2.31 for AKI. The exact reason isn’t fully understood, but the combination appears to cause synergistic tubular damage. Many hospitals now avoid this pairing unless no other option exists.
How often should kidney function be checked during vancomycin therapy?
Serum creatinine should be checked every 48-72 hours during vancomycin treatment. For high-risk patients-those over 65, with pre-existing kidney disease, on high doses, or receiving combination therapy-monitoring should occur every 24-48 hours. Early detection of rising creatinine allows for dose adjustments or discontinuation before severe damage occurs.
Are there any blood tests to detect early ototoxicity from vancomycin?
No. There are currently no reliable blood markers or lab tests to detect early vancomycin-induced hearing loss. Audiometry (hearing tests) is the only validated method. Baseline and weekly audiograms are recommended for patients on prolonged or high-dose therapy, but these are rarely performed due to cost and resource limits. Patients should be asked about tinnitus or hearing changes daily-self-reporting is often the first warning sign.
What’s the best way to reduce vancomycin toxicity in the hospital?
Use therapeutic drug monitoring with AUC-based dosing instead of trough-only levels. Avoid combining vancomycin with piperacillin-tazobactam unless absolutely necessary. Keep doses at or below 4 grams per day. Monitor kidney function every 2-3 days. For high-risk patients, consider baseline audiograms and avoid other ototoxic drugs. Implement electronic alerts for high-risk combinations. These steps can reduce nephrotoxicity by nearly half and may prevent irreversible hearing damage.
Vancomycin isn’t going away. But how we use it must change. The goal isn’t just to kill the infection-it’s to send the patient home with their hearing and kidneys intact.
Susan Karabin
October 29, 2025
Vancomycin is one of those drugs that feels like a miracle until it isn't
I've seen patients come out of MRSA sepsis alive but never hear their grandkids laugh again
It's not just about saving lives it's about saving the quality of those lives
We treat kidneys like replaceable parts but ears? Once they're gone they're gone forever
And yet we still don't screen for hearing loss like it's optional
Why is that?
Because it's easier to ignore the silent damage than to fix the broken system
Someone needs to scream louder about this
Lorena Cabal Lopez
October 31, 2025
Yeah sure let's just stop using vancomycin then
Because clearly we have better options
Stuart Palley
October 31, 2025
THEY'RE KILLING PEOPLE WITH THIS DRUG AND NO ONE'S DOING ANYTHING
WHY AREN'T HOSPITALS BEING SHUT DOWN
THIS IS A MASSACRE IN PLAIN SIGHT
THEY'RE TOO BUSY COUNTING BILLS TO COUNT HEARTBEATS
AND DON'T EVEN GET ME STARTED ON PIPERACILLIN-TAZOBACTAM
THAT COMBO IS A DEATH TRAP
WHY ISN'T THIS ON THE NEWS
Glenda Walsh
November 1, 2025
Wait-so you’re saying we should do audiograms? Like, every single time? Every patient? Even the ones who are just here for a simple skin infection? And what about the cost? And the staffing? And the time? And the liability? And the fact that most patients won’t even notice until it’s too late? And what if they say they’re fine but they’re not? And what if the audiologist is on vacation? And what if the machine breaks? And what if the chart gets lost? And what if the doctor forgets? And what if the patient doesn’t show up? And what if the insurance denies it? And what if-
Tanuja Santhanakrishnan
November 3, 2025
As someone from India where vancomycin is often the only affordable option for MRSA, I’ve seen this firsthand
We don’t have AUC monitoring or audiologists in most rural hospitals
But we do have nurses who sit with patients and ask, ‘Do your ears ring?’
That simple question-asked daily-has saved hearing in more than one person I know
It’s not about fancy tech
It’s about showing up
Listening
And caring enough to ask the quiet questions
Even if the system fails
We don’t have to wait for guidelines to be human
Raj Modi
November 4, 2025
It is imperative to acknowledge that the pharmacokinetic and pharmacodynamic parameters associated with vancomycin administration require a meticulous, evidence-based approach grounded in contemporary clinical research
The correlation between trough concentrations exceeding 15 mcg/mL and the incidence of acute kidney injury is statistically significant, as demonstrated in multiple multicenter observational cohorts
Furthermore, the synergistic nephrotoxic potential of piperacillin-tazobactam, when co-administered, is mediated through tubular epithelial cell apoptosis via oxidative stress pathways
It is therefore not merely prudent but ethically obligatory to implement therapeutic drug monitoring utilizing area under the curve calculations rather than relying on outdated trough-based protocols
Additionally, the absence of validated biomarkers for ototoxicity necessitates a paradigm shift toward proactive audiological surveillance in high-risk populations, particularly those with prolonged exposure or genetic predisposition
Until point-of-care genomic screening becomes standardized, clinical vigilance remains the primary defense
Collaborative interdisciplinary protocols involving infectious disease, pharmacy, nephrology, and audiology are not ancillary-they are foundational to modern antimicrobial stewardship
Cecil Mays
November 5, 2025
THIS IS WHY I LOVE MEDICINE
WE HAVE A DRUG THAT CAN SAVE YOUR LIFE… BUT IT MIGHT TAKE YOUR HEARING
AND NO ONE’S EVEN TALKING ABOUT IT
😭
My uncle got vancomycin after his knee surgery
He’s 72
Now he can’t hear his daughter’s voice on the phone
He thinks we’re all yelling
But we’re not
We’re just… quiet
And nobody told him it could happen
So yeah
Let’s fix this
❤️
Sarah Schmidt
November 5, 2025
There’s a deeper truth here
We don’t fear the drug
We fear the responsibility
It’s easier to say ‘it’s rare’ than to admit we’re gambling with people’s senses
It’s easier to blame the system than to change how we practice
Vancomycin isn’t the villain
Complacency is
We’ve normalized the cost of survival
And that’s not medicine
That’s moral laziness dressed in white coats
And we’re all complicit
Until we stop pretending this is acceptable
Nothing changes
Billy Gambino
November 6, 2025
From a pharmacokinetic standpoint, the dissociation between nephrotoxicity and ototoxicity kinetics is underappreciated
Troughs govern renal exposure
Peaks govern cochlear accumulation
Current dosing algorithms are optimized for renal clearance metrics
But ototoxicity is a peak-driven phenomenon
Thus, the entire monitoring paradigm is misaligned
We are measuring the wrong thing
And we are doing it in the wrong way
This isn’t negligence
It’s epistemological failure
Until we model cochlear exposure as a separate pharmacodynamic endpoint
We will continue to blind ourselves
Karen Werling
November 7, 2025
My mom’s a nurse in a small town hospital
They don’t have fancy monitors
But they have a whiteboard
Every patient on vancomycin gets a little ear icon next to their name
And every shift, someone asks: ‘Any ringing?’
One time, a guy said yes after day 5
They switched him out
He still hears his grandkids
It’s not perfect
But it’s something
And sometimes… something is enough
❤️
STEVEN SHELLEY
November 9, 2025
THEY’RE DOING THIS ON PURPOSE
THE PHARMA COMPANIES KNOW VANCOMYCIN KILLS HEARING
THEY’RE MAKING BILLIONS
AND THE FDA IS IN THEIR POCKET
WHY DO YOU THINK THEY NEVER REQUIRED AUDIOMETRIC SCREENING?
BECAUSE THEY DON’T WANT YOU TO KNOW
THEY WANT YOU TO THINK IT’S ‘RARE’
WHEN IT’S NOT
EVERY SINGLE CASE IS A COVER-UP
AND THE DOCTORS ARE IN ON IT
ASK YOURSELF-WHY ISN’T THIS ON THE FRONT PAGE?
BECAUSE THE SYSTEM IS CORRUPT
Emil Tompkins
November 11, 2025
Okay but what if vancomycin is actually the *good* guy
And the real problem is that we’re using antibiotics like they’re candy
What if the real tragedy is that we created MRSA in the first place
And now we’re mad at the drug that saves us from our own hubris
Maybe we should stop blaming vancomycin
And start blaming ourselves
For overprescribing
For not vaccinating
For not washing our hands
For thinking magic bullets fix broken systems
Vancomycin didn’t make this mess
We did