Ranitidine Bone Health Risk Estimator
Personalized Risk Assessment
This tool estimates your osteoporosis risk based on ranitidine use and key factors.
When you hear the name Ranitidine is a histamine H2‑receptor antagonist that reduces stomach acid, the first thing that probably comes to mind is heartburn relief. But a growing body of research suggests the drug might have a hidden impact on your bones. This article unpacks the science, weighs the evidence, and tells you what to do if you’re taking ranitidine and worrying about osteoporosis.
Key Takeaways
- Ranitidine lowers stomach acid, which can impair calcium absorption over long‑term use.
- Observational studies link chronic ranitidine therapy to modest reductions in bone mineral density (BMD) and a slight rise in fracture risk.
- The FDA’s 2024 recall of ranitidine due to NDMA contamination has shifted focus to safer alternatives, but the bone‑health question remains.
- Patients at high fracture risk should discuss bone‑protective strategies-diet, supplements, or switching medications-with their doctor.
- Evidence for a direct cause‑and‑effect link is still inconclusive; the safest path is regular monitoring and lifestyle support.
What Is Ranitidine and How Does It Work?
Ranitidine belongs to the class of Histamine H2 blockers. It blocks histamine receptors in the stomach lining, curbing the production of gastric acid. The drug became a go‑to for conditions like gastroesophageal reflux disease (GERD) and peptic ulcer disease, offering an over‑the‑counter alternative to prescription‑only proton pump inhibitors (PPIs).
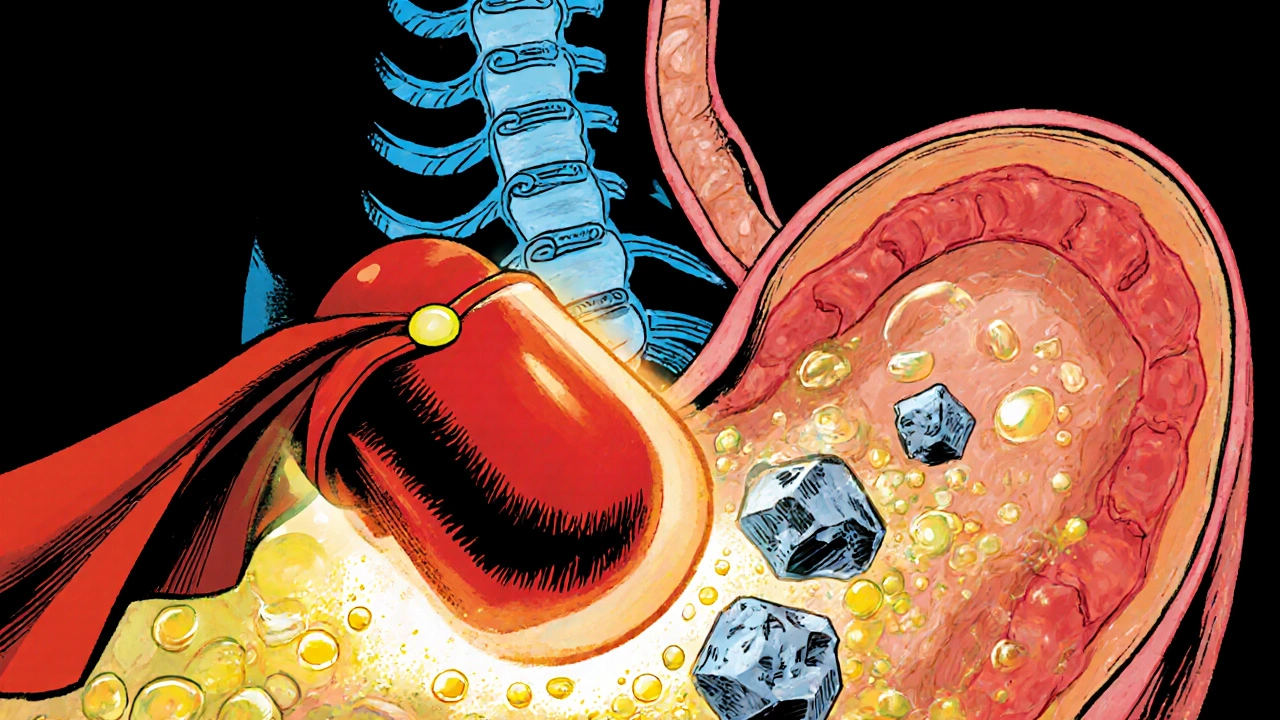
Why Bone Health Enters the Picture
The connection between stomach acid and bone health might sound odd, but it’s rooted in calcium chemistry. Calcium carbonate-one of the most common calcium supplements-needs an acidic environment to dissolve properly. When ranitidine suppresses acid, the body may absorb less calcium from food and supplements. Over months or years, this shortfall can chip away at Bone mineral density, the key metric doctors use to diagnose Osteoporosis.
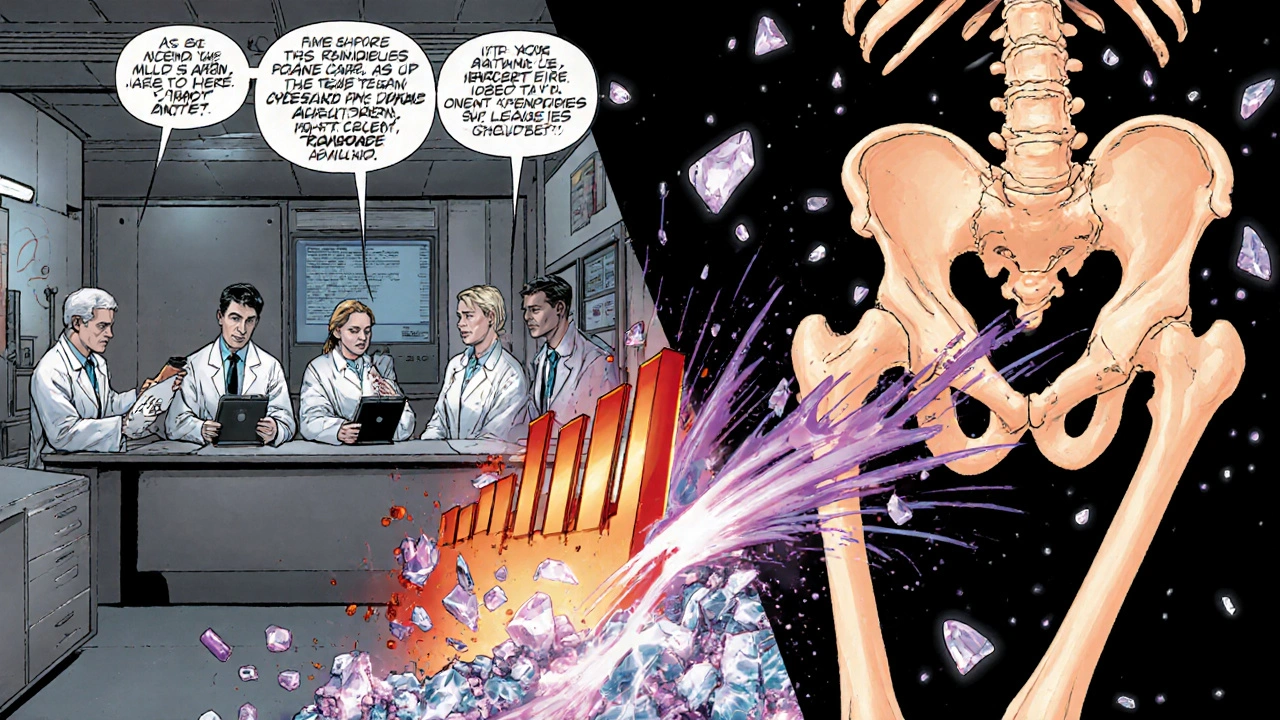
What the Studies Say
Research on ranitidine and bone health falls into three buckets:
- Observational Cohorts: Large database analyses from the UK and US (e.g., a 2022 cohort of 45,000 ranitidine users) reported a 7‑12% higher incidence of hip fractures after five years of continuous use, compared with non‑users.
- Mechanistic Trials: Small crossover trials measuring calcium absorption showed a 15‑20% drop in fractional calcium uptake after two weeks of high‑dose ranitidine, but the effect faded once the drug was stopped.
- Comparative Reviews: Systematic reviews published in 2023 concluded that H2 blockers, including ranitidine, carry a modest fracture risk-lower than PPIs but still statistically significant versus no acid‑suppressing therapy.
None of these studies prove causation, but the pattern is consistent enough to raise a red flag for clinicians.
Regulatory Action and the NDMA Issue
In 2024 the FDA announced a nationwide recall of all ranitidine products after detecting N‑nitrosodimethylamine (NDMA), a probable human carcinogen, in several batches. While NDMA concerns dominate headlines, the recall also sparked renewed scrutiny of the drug’s broader safety profile, including bone health. The recall has pushed many prescribers to switch patients to either other H2 blockers (like famotidine) or PPIs, each with its own bone‑risk profile.
How Does Ranitidine Compare to Other Acid‑Suppressors?
| Medication | Mechanism Related to Calcium | Typical Effect on BMD (5‑Year Data) | Relative Fracture Risk |
|---|---|---|---|
| Ranitidine (H2 blocker) | Reduces gastric acid → modestly lowers calcium carbonate solubility | -1.5% to -2.5% (small but measurable) | 1.07‑1.12× (7‑12% increase) |
| Proton Pump Inhibitors (e.g., omeprazole) | Strong acid suppression → greater impact on calcium absorption | -3% to -5% | 1.20‑1.30× (20‑30% increase) |
| None (no acid‑suppressor) | Normal gastric pH → optimal calcium dissolution | Stable or slight gain (+0.3% to +0.5%) | Baseline (1.0×) |
The table shows that ranitidine’s bone‑health impact sits between PPIs and no medication. If you need an acid‑suppressor, the choice matters for long‑term skeletal health.
Who Is Most at Risk?
Not everyone on ranitidine will develop osteoporosis. The highest‑risk groups include:
- Post‑menopausal women - naturally lower estrogen and already higher fracture rates.
- Older adults (≥65years) - age‑related bone loss accelerates any medication‑induced deficit.
- Patients with chronic kidney disease - impaired calcium‑phosphate balance makes them vulnerable.
- Those on concurrent steroids or bisphosphonate‑sparing regimens - additive bone‑loss factors.
If you fall into any of these categories, a proactive approach is worth the effort.
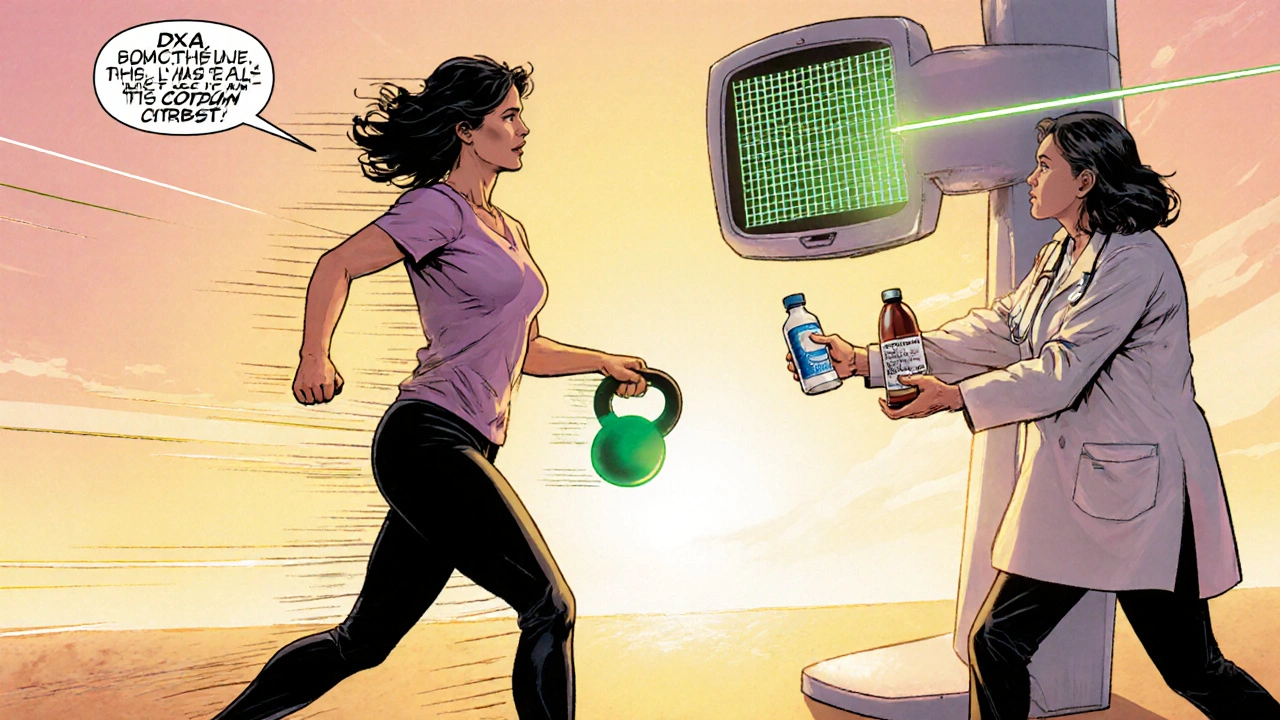
Practical Steps to Protect Your Bones
- Ask Your Doctor About Alternatives: Famotidine appears to have a milder effect on calcium absorption, and some newer PPIs can be tapered or given on-demand rather than full‑time.
- Monitor Bone Density: A dual‑energy X‑ray absorptiometry (DXA) scan every 2‑3years provides a baseline and tracks changes.
- Boost Calcium and Vitamin D: Aim for 1,200mg of calcium (preferably from dairy, leafy greens, or calcium citrate-a form less dependent on acid) and 800-1,000IU of vitamin D daily.
- Stay Active: Weight‑bearing exercises-walking, light resistance training, or dancing-stimulate bone formation.
- Limit Alcohol and Quit Smoking: Both habits accelerate bone loss and compound any medication effect.
Adopting these habits can offset a modest medication‑related risk.
When to Seek Professional Advice
If you experience any of the following, schedule a check‑up:
- Unexpected back, hip, or wrist pain after a minor fall.
- Loss of height or a stooped posture over a few months.
- Repeated short‑term courses of ranitidine (more than 3months total) without a clear plan to stop.
A clinician can evaluate your fracture risk using tools like FRAX, order a DXA scan, and discuss whether a calcium supplement or prescription bisphosphonate is appropriate.
Bottom Line
Ranitidine does not cause osteoporosis overnight, but long‑term use can shave a few points off bone density by hindering calcium absorption. The risk is real but modest, and it sits below the bone‑health concerns tied to PPIs. For most people, the best strategy is regular monitoring, a calcium‑rich diet, and a conversation with your healthcare provider about whether a switch to a different medication is warranted.
Frequently Asked Questions
Does taking ranitidine increase my chance of breaking a bone?
Observational data suggest a 7‑12% higher risk of hip or vertebral fractures after five years of continuous use. The increase is modest and often outweighed by other risk factors like age and vitamin D status.
Can I safely take calcium carbonate supplements while on ranitidine?
Calcium carbonate needs stomach acid to dissolve. If you stay on ranitidine, consider calcium citrate instead-it’s absorbed well even with reduced acidity.
Is famotidine a better choice for bone health?
Current evidence points to famotidine having a slightly lower impact on calcium absorption than ranitidine, though data are limited. It’s generally considered a safer H2 blocker for long‑term users concerned about bone loss.
Should I get a bone‑density scan if I’ve been on ranitidine for a few months?
A DXA scan is most useful for people with other risk factors (age >65, menopause, steroid use). For short‑term users without additional risks, routine scanning isn’t usually recommended.
What other medications can affect bone health?
Long‑term use of PPIs, glucocorticoids, certain anticonvulsants, and thiazide diuretics can all influence calcium balance or bone remodeling. Always discuss medication combos with your doctor.
Tushar Agarwal
August 13, 2025
Great summary, really helped me understand the link between ranitidine and bone health! 😊
Richard Leonhardt
August 17, 2025
Glad it was useful! Just a heads‑up, you might see my name spelled "Richrd" in some older papers, but the data stays the same.
Shaun Brown
August 21, 2025
It's astonishing how many laypeople trivialize the ranitidine‑osteoporosis connection. The article glosses over the mechanistic trials, which actually showed a 20% dip in calcium absorption after just two weeks. Yet you read my earlier comment and think the risk is negligible. The data from the UK cohort of 45,000 users is not "just an association". It demonstrates a statistically significant 7‑12% boost in fracture rates that cannot be dismissed as noise. Moreover, the recall due to NDMA only scratches the surface of the drug's safety profile. The fact that famotidine may have a milder impact doesn't absolve ranitidine of its own culpability. Patients over 65, especially post‑menopausal women, are a demographic that should be screaming for alternative therapy. The article's recommendation to "stay on calcium supplements" feels like a half‑hearted band‑aid. Most supplements rely on calcium carbonate, which needs an acidic stomach to dissolve-exactly what ranitidine suppresses. Switching to calcium citrate is prudent, but the piece fails to stress that enough. Likewise, the suggestion to get a DXA scan every 2‑3 years is good advice, but why wait until after years of exposure? Proactive monitoring would catch bone density loss earlier and possibly spare patients from painful fractures. The tone of the article is overly reassuring, bordering on complacency. If you truly care about patient outcomes, you would champion a more aggressive medication review. In short, the risk is real, the evidence is solid, and the medical community should act accordingly.
Damon Dewey
August 25, 2025
Stop sugar‑coating a drug that silently robs you of bone.
Dan Barreto da Silva
August 29, 2025
OMG, can you imagine taking ranitidine for years and then finding out your bones are whispering for help? It's like a thriller where the villain is a heartburn pill! 😱
Ariel Munoz
September 2, 2025
Seriously, this whole ranitidine hype is just pharma propaganda. In our country we prefer proven remedies, not these questionable blockers.
Ryan Hlavaty
September 6, 2025
We should all demand transparency from drug manufacturers. If a medication can jeopardize bone health, the public deserves to know before swallowing a pill.
Chris Faber
September 10, 2025
I've been using a H2 blocker for a while and haven't felt any bone issues yet, but I do keep an eye on my calcium intake and try to stay active.
aura green
September 14, 2025
Wow, because nothing says "I'm responsible adult" like Googling a 2024 FDA recall at 2 am and then panicking about my hip joint. 🙄 It's adorable how everyone suddenly becomes a bone health guru after reading a few bullet points. Sure, calcium carbonate might be less effective, but have you tried actually eating dairy? And if you’re worried, just schedule a DXA scan-because who doesn’t love a good X‑ray for fun? Meanwhile, the rest of us will keep taking our meds and sipping water, hoping the universe doesn’t decide to steal our femur.
Edward Morrow
September 18, 2025
Enough with the milk‑toast optimism-ranitidine is a sneaky calcium‑stealer that can turn your skeleton into a house of cards. If you don’t ditch it, you’re practically signing a death‑by‑fracture contract.
Shayne Tremblay
September 22, 2025
Hey folks! If you’re on ranitidine, don’t panic-just boost your calcium intake with foods like kale and almonds, and squeeze in some sunshine for vitamin D. A little walk or jog each day can do wonders for bone strength, too!
Stephen Richter
September 27, 2025
While enthusiasm is valuable, clinical data should guide supplementation decisions
Musa Bwanali
October 1, 2025
Listen, the key is consistency-track your calcium, get that DXA scan on schedule, and keep moving. That’s how you win the bone battle.
Allison Sprague
October 5, 2025
Spelling mistakes aside, the article's claims are riddled with vague qualifiers. "May reduce" and "could increase" are not scientific; they’re filler. Readers deserve precise statistics, not wishful prose.
leo calzoni
October 9, 2025
In truth, the evidence is clear: ranitidine poses a measurable bone risk.
KaCee Weber
October 13, 2025
🌟 I love how this piece pulls together data from cohorts, trials, and real‑world recalls-it's a solid foundation for anyone questioning their medication. 🦴 Remember that calcium citrate works well even if stomach acid is low, so switching supplements can mitigate the issue. 🍊 Vitamin D sunshine is non‑negotiable; aim for 15‑20 minutes daily if you can. 📅 And don’t forget to schedule that bone density scan, especially if you’re over 65 or have other risk factors. 🏃♀️ Staying active with weight‑bearing exercises like dancing or resistance training will keep those bones happy. 🎉 Bottom line: awareness plus a few lifestyle tweaks can offset the modest risk from ranitidine.
jess belcher
October 17, 2025
Overall, informed choices and regular monitoring are the best tools we have to protect bone health while managing acid reflux