Fluid Restriction Calculator for Hydrochlorothiazide
Personalized Fluid Restriction Calculator
Helping you maintain good sleep quality while taking Hydrochlorothiazide by calculating the right fluid limits after dinner.
Enter your information above to see your personalized fluid restriction recommendation.
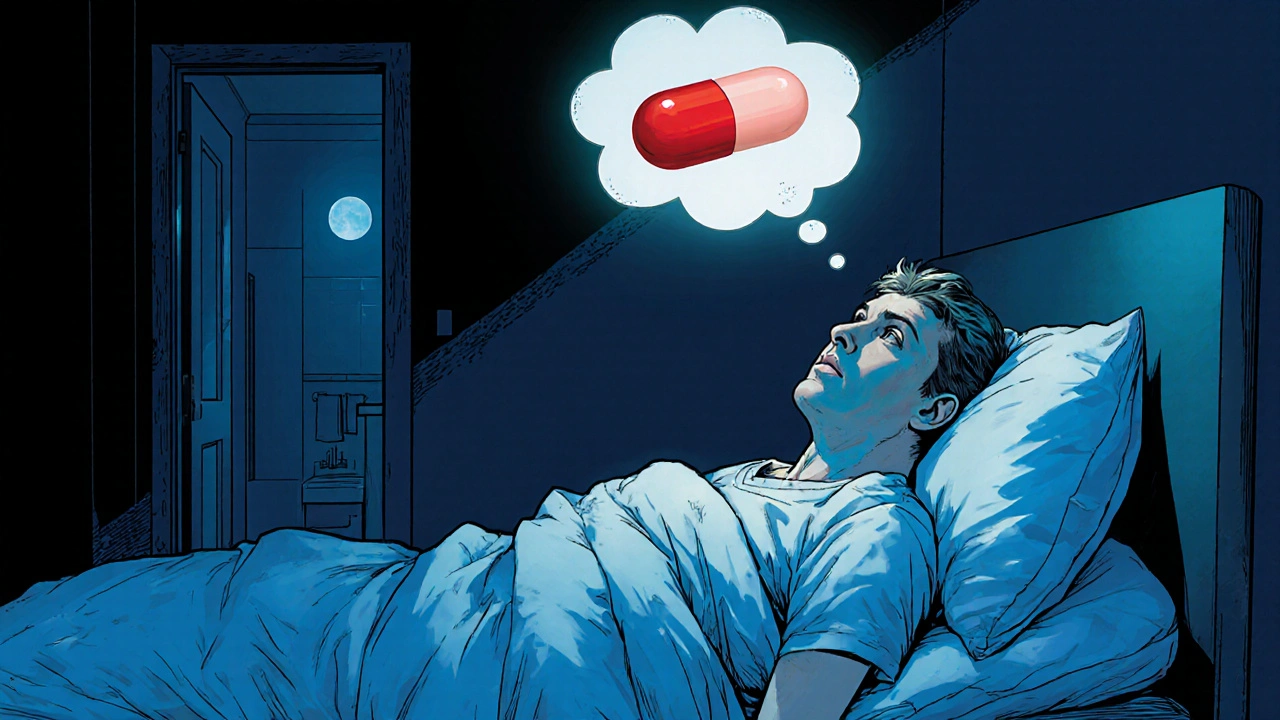
When you hear the name Hydrochlorothiazide is a thiazide diuretic commonly prescribed for hypertension and fluid retention, you probably think of blood pressure numbers, not bedtime. Yet many patients report waking up thirsty, needing the bathroom, or feeling restless after starting the pill. This article unpacks whether Hydrochlorothiazide sleep issues are real, how the drug works, and what you can do to protect your sleep quality.
Key Takeaways
- Hydrochlorothiazide can increase nighttime trips to the bathroom (nocturia) because it makes you pee more.
- Changes in potassium and sodium levels may trigger muscle cramps or restlessness that disturb sleep.
- Taking the dose in the morning and limiting fluids after noon often reduces sleep disruption.
- If you notice persistent insomnia, vivid dreams, or severe electrolyte symptoms, talk to your doctor about dosing time or a different diuretic.
- Simple sleep‑hygiene tweaks-cool bedroom, consistent schedule, and proper hydration-work hand‑in‑hand with medication management.
How Hydrochlorothiazide Works
Hydrochlorothiazide blocks sodium reabsorption in the distal convoluted tubule of the kidney. By keeping more sodium in the urine, water follows, which lowers blood volume and, consequently, blood pressure. The drug’s half‑life is roughly 6‑15hours, meaning its diuretic effect can linger well into the evening if taken later in the day.
Sleep‑Related Side Effects to Watch For
Most side effects are listed on the medication label, but a few have a direct line to sleep quality:
- Nocturia: The most common culprit. Increased urine production may force you to the bathroom 1‑3 times a night, breaking deep sleep cycles.
- Electrolyte imbalance: Thiazides can lower potassium and raise calcium. Low potassium (hypokalemia) often shows up as leg cramps or restless legs, both of which can keep you tossing.
- Blood‑pressure fluctuations: A sudden dip in pressure when you stand up (orthostatic hypotension) can cause light‑headedness or a racing heart, both unsettling at bedtime.
- Insomnia or vivid dreams: Though rare, some users report trouble falling asleep or unusually vivid dreams, possibly linked to shifts in hydration and electrolyte status.
Who Is Most Susceptible?
Not everyone on Hydrochlorothiazide will notice sleep problems. The risk rises if you fall into one of these groups:
- Older adults: Kidney function naturally declines with age, slowing drug clearance and exaggerating nocturnal urine output.
- High daily dose: Doses above 25mg are more likely to cause pronounced diuresis.
- People who drink fluids after dinner: Evening coffee, tea, or even a glass of water can amplify the drug’s effect.
- Patients with pre‑existing electrolyte issues: Those on other potassium‑lowering meds (e.g., certain antibiotics) may feel cramps sooner.
Practical Tips to Protect Your Sleep
Below are easy‑to‑implement strategies that many patients find helpful.
- Morning dosing: Take Hydrochlorothiazide with breakfast or early lunch. This aligns its peak effect with daytime activity, allowing the excess fluid to be expelled before bedtime.
- Limit evening fluids: Aim to finish most of your daily water intake by 6p.m. If you’re thirsty after that, sip a small amount of water and keep a bathroom nearby.
- Potassium‑rich foods: Include bananas, oranges, spinach, and avocados in your dinner. For some patients, a low‑dose potassium supplement (under doctor’s guidance) can stave off cramps.
- Sleep‑hygiene basics: Keep the bedroom cool (around 65°F/18°C), dim the lights an hour before bed, and avoid screens that emit blue light.
- Mind the timing of other meds: Certain antihypertensives (e.g., ACE inhibitors) taken at night can offset the blood‑pressure dip caused by Hydrochlorothiazide, smoothing out nighttime fluctuations.
Alternative Diuretics and Timing Strategies
If morning dosing doesn’t solve the problem, discuss alternatives with your clinician. The table below compares the two most common thiazide‑type diuretics regarding their impact on sleep.
| Drug | Typical Dose | Half‑Life | Nocturia Risk | Electrolyte Effect |
|---|---|---|---|---|
| Hydrochlorothiazide | 12.5‑50mg daily | 6‑15h | Medium‑High | ↓K⁺, ↑Ca²⁺ |
| Chlorthalidone | 12.5‑25mg daily | 40‑60h | Low‑Medium (longer acting, less nighttime spike) | ↓K⁺, ↑Ca²⁺ (similar) |
Chlorthalidone’s longer half‑life spreads the diuretic effect more evenly, often resulting in fewer nighttime bathroom trips. However, its strong potassium‑lowering effect means you might still need supplementation.
When to Talk to Your Doctor
Sleep disruption that persists beyond a couple of weeks, or any of the following symptoms, merit a call:
- More than two nightly trips to the bathroom despite fluid restriction.
- Severe muscle cramps, weakness, or irregular heartbeat (signs of hypokalemia).
- Persistent insomnia, vivid nightmares, or daytime fatigue.
- Sudden drop in blood pressure causing dizziness or fainting.
Your clinician may adjust the dose, shift the timing, prescribe a potassium‑sparing diuretic, or explore a completely different class of antihypertensives.
Bottom Line
Hydrochlorothiazide isn’t a sleep‑killer by design, but its diuretic action can disturb nighttime rest, especially if taken later in the day or combined with high fluid intake. By mastering dose timing, watching electrolytes, and practicing solid sleep hygiene, most people can keep both their blood pressure and sleep quality in good shape.
Frequently Asked Questions
Can Hydrochlorothiazide cause insomnia?
Insomnia is not a listed side effect, but the frequent nighttime urination and electrolyte‑related leg cramps it can cause often interrupt sleep, making it feel like the medication is the direct culprit.
Is it safe to take Hydrochlorothiazide in the evening?
Evening dosing is possible, but it raises the chance of nocturia. Most clinicians recommend a morning dose unless your blood‑pressure pattern specifically calls for a nighttime schedule.
How much fluid should I avoid after dinner?
A practical rule is to stop drinking anything >150ml (about 5oz) after 6p.m. If you’re thirsty, sip a small glass of water and keep the bathroom light on.
Do potassium supplements interfere with Hydrochlorothiazide?
They can help counteract low potassium, but only take them under a doctor’s guidance. Excess potassium can lead to its own heart rhythm problems.
Are there other diuretics that don’t affect sleep?
Long‑acting thiazides like chlorthalidone or potassium‑sparing agents (e.g., spironolactone) tend to produce fewer nighttime bathroom trips, but each has its own side‑effect profile. Discuss options with your prescriber.
Emily Collier
October 15, 2025
Hydrochlorothiazide can indeed increase nocturnal bathroom trips, so timing the dose earlier in the day often helps. Pairing the medication with potassium‑rich foods may reduce cramp‑related awakenings. Also, keeping the bedroom cool and limiting fluids after dinner are simple sleep‑hygiene steps. If problems persist, a brief consult with your provider is advisable.
Catherine Zeigler
October 19, 2025
Many patients find that the half‑life of hydrochlorothiazide, which stretches from six to fifteen hours, overlaps with their evening routine, prompting unwanted trips to the bathroom. Shifting the dose to breakfast aligns the peak diuretic effect with daytime activity, allowing excess fluid to be eliminated before bedtime. This simple adjustment can dramatically improve sleep continuity for a large portion of the population. Additionally, monitoring electrolyte balance is crucial; low potassium often manifests as restless legs or nocturnal cramps that further disrupt sleep. Incorporating potassium‑rich foods such as bananas, oranges, spinach, and avocados into dinner can mitigate these symptoms without the need for supplemental pills, provided you have no contraindications. If you are already on a high‑dose regimen-say, above 25 mg daily-the likelihood of nocturia rises, making dose reduction a reasonable first step. For older adults, reduced kidney clearance amplifies the drug’s duration, so a lower dose or a switch to a longer‑acting thiazide like chlorthalidone may be advantageous. Limiting fluid intake after 6 p.m. does not mean you must dehydrate; a small sip of water is acceptable, but avoid coffee, tea, or large glasses of water late at night. Establishing a consistent bedtime schedule helps entrain the circadian rhythm, making it easier to fall asleep even if occasional bathroom trips occur. Dim the lights an hour before bed and keep electronic devices away to reduce blue‑light exposure, which can further enhance sleep quality. If you notice vivid dreams or insomnia that you suspect are medication‑related, keep a sleep diary for two weeks to document patterns before discussing changes with your doctor. In some cases, a potassium‑sparing diuretic, such as spironolactone, can be added to offset hypokalemia while preserving antihypertensive efficacy. Always review any supplement or medication change with your healthcare provider to avoid dangerous electrolyte shifts. Remember that lifestyle factors-exercise, stress management, and a cool bedroom environment-work synergistically with pharmacologic adjustments. By combining thoughtful dosing, electrolyte awareness, and solid sleep hygiene, most individuals can maintain both healthy blood pressure and restorative sleep.
henry leathem
October 23, 2025
The diuretic effect of HCTZ is not a trivial footnote; it directly escalates nocturnal polyuria, which undermines sleep architecture. If you’re not adjusting your fluid window, you’re essentially sabotaging your own rest.
jeff lamore
October 27, 2025
Taking hydrochlorothiazide earlier in the day aligns its peak action with waking hours, reducing the need for late‑night bathroom trips. Pairing it with a modest potassium supplement can blunt muscle cramps that otherwise cause tossing. Maintaining a consistent sleep schedule further stabilizes blood pressure fluctuations at night.
Kris cree9
October 31, 2025
OMG this med totally wrecks my sleep!
Paula Hines
November 4, 2025
One could argue that the pharmacokinetic profile of hydrochlorothiazide justifies a reconsideration of dosing schedules; however, the prevailing clinical guidelines often overlook patient‑centric sleep outcomes. It is incumbent upon us to examine the intersection of electrolyte homeostasis and nocturnal arousals, especially in populations predisposed to hypokalemia. By integrating potassium‑rich dietary sources, we may attenuate leg cramps without resorting to additional pharmacotherapy. Moreover, the temporal distribution of fluid intake remains a modifiable variable that can be tailored to individual circadian rhythms. Ultimately, a collaborative dialogue between prescriber and patient is essential to optimize both antihypertensive efficacy and sleep quality.
John Babko
November 7, 2025
Excellent point, Jeff! Timing is everything, especially with a diuretic that can linger for hours, so a morning dose clears the system before bedtime, reducing nocturia, and the added potassium helps prevent cramps, which are a major sleep disruptor, right?
Stacy McAlpine
November 11, 2025
Different cultures have varied approaches to nighttime hydration, but the science is clear: less fluid after dinner means fewer bathroom trips. Try swapping late‑night coffee for herbal tea and see the difference.
Roger Perez
November 14, 2025
Totally agree! 🙌 Keeping the lights dim and a water bottle nearby works wonders. 😴
michael santoso
November 18, 2025
While the layperson may attribute any insomnia to the medication, a rigorous analysis reveals that confounding variables such as comorbid anxiety disorders often play a more substantial role. Consequently, attributing causality solely to hydrochlorothiazide without controlling for these factors is intellectually careless. A nuanced, evidence‑based approach is required for any meaningful clinical recommendation.
M2lifestyle Prem nagar
November 21, 2025
Take your dose early, limit fluids after six. Simple changes improve sleep.
Karen Ballard
November 25, 2025
Good tip! 😊👍