When a new medication hits the market, the excitement about its therapeutic promise often overshadows the tough moral questions that come with it. Aciderm is no exception. This article breaks down the biggest ethical dilemmas surrounding Aciderm, from safety testing to who actually gets to afford it, and offers a practical checklist for anyone involved in its rollout.
What is Aciderm?
Aciderm is a novel oral medication designed to treat chronic gastric acidity disorders. Developed by GastroPharm Inc., it received provisional approval from the U.S. Food and Drug Administration (FDA) in early 2024 after showing a 42% reduction in symptom severity in PhaseIII trials.
While the drug promises faster relief than existing proton‑pump inhibitors, its mechanism-targeting a newly discovered acid‑secreting pathway-raises fresh questions about long‑term effects, especially in vulnerable populations.
Core ethical principles in drug development
Any discussion of drug ethics starts with the four pillars of biomedical ethics:
- Beneficence: Do the benefits outweigh the risks?
- Non‑maleficence: Avoid causing harm.
- Autonomy: Respect patients’ right to make informed choices.
- Justice: Ensure fair distribution of benefits and burdens.
These principles apply at every stage-from pre‑clinical animal work to post‑marketing surveillance-so we’ll use them as a lens to examine Aciderm’s journey.
Safety and risk assessment of Aciderm
Aciderm’s safety profile looks promising on paper: common adverse events were mild nausea (12%) and transient headache (8%). However, three serious cases of liver enzyme elevation were reported, sparking debate about whether the trial size was sufficient to catch rare but severe toxicities.
Key ethical concerns include:
- Sample representativeness: The pivotal trials enrolled primarily healthy adults aged 18‑55. Older patients, who represent a large share of acid‑related disease, were under‑represented, making it hard to gauge risk in that group.
- Long‑term monitoring: The drug targets a novel pathway that could affect nutrient absorption. Current post‑marketing studies are limited to one year, potentially missing chronic effects.
- Transparency of data: GastroPharm has released only summary data. Independent researchers call for raw trial datasets to conduct independent meta‑analyses.
Ethically, regulators and sponsors should expand surveillance, mandate real‑world evidence collection, and open data to the scientific community.
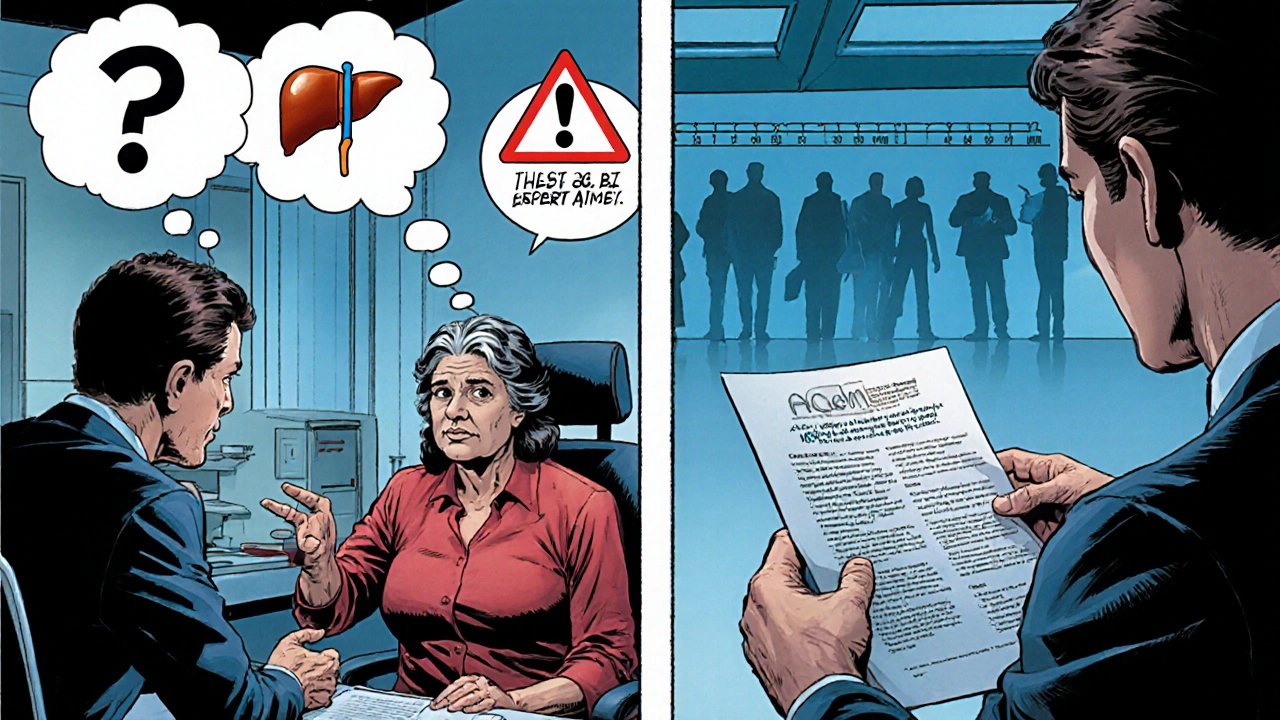
Informed consent and patient autonomy
When doctors prescribe Aciderm, patients must understand both its benefits and unknowns. Yet consent forms often gloss over uncertainties, focusing on the drug’s efficacy.
Consider the following scenario: Maria, a 62‑year‑old with a history of liver disease, asks whether Aciderm is safe for her. The clinician, pressed for time, says, “It’s approved, so it’s fine.” This short‑change of autonomy violates the ethical duty of informed consent.
To protect autonomy, consent materials should include:
- Clear language about the drug’s novel mechanism.
- Explicit statements about what is unknown-especially long‑term liver safety.
- Alternative treatment options and why a patient might prefer them.
Embedding these points respects the patient’s right to decide based on full information.
Access, affordability, and equity
Aciderm’s price tag-$250 for a month’s supply-places it out of reach for many uninsured or under‑insured patients. This raises a classic justice issue: should a drug that offers incremental improvement be priced at premium levels?
Stakeholders can address equity by:
- Negotiating with insurers for tiered copays based on income.
- Creating patient‑assistance programs for low‑income groups.
- Ensuring generic competition enters the market within 5‑7 years, as mandated by U.S. law.
Without these measures, the drug could widen health disparities, benefitting only those who can afford it.
Off‑label use and marketing practices
Early after launch, some gastroenterologists began prescribing Aciderm for non‑acid‑related conditions like functional dyspepsia, citing anecdotal improvements. Pharmaceutical companies have a history of promoting off‑label uses to boost sales, which can erode trust.
Ethical marketing should:
- Disclose that off‑label efficacy is not yet proven.
- Avoid incentive payments for prescribing the drug for unapproved indications.
- Submit rigorous clinical data before expanding the label.
Violating these norms can lead to legal penalties and, more importantly, patient harm.
Regulatory landscape and oversight
The FDA’s “accelerated approval” pathway allowed Aciderm to reach the market based on surrogate endpoints (acid reduction) rather than hard outcomes (ulcer healing). While this speeds access, it also transfers more post‑approval risk to the public.
Key regulatory responsibilities include:
- Requiring post‑marketing PhaseIV trials that measure long‑term clinical outcomes.
- Monitoring adverse event reports through the FDA’s FAERS database and acting quickly on safety signals.
- Enforcing transparent labeling that highlights known uncertainties.
For clinicians, staying updated on FDA safety communications is essential to uphold ethical prescribing.

Practical ethical checklist for stakeholders
Below is a quick reference anyone involved with Aciderm can use to keep ethical considerations front‑and‑center.
| Stage | Key Ethical Question | Action Item |
|---|---|---|
| Pre‑clinical | Are animal studies designed to minimize suffering? | Follow ARRIVE guidelines; use alternatives when possible. |
| Clinical trials | Is the participant pool diverse enough? | Recruit older adults and patients with comorbidities. |
| Regulatory review | Do surrogate endpoints adequately reflect patient benefit? | Request additional outcome data before full approval. |
| Prescribing | Has the patient been fully informed of uncertainties? | Provide concise consent sheets highlighting unknowns. |
| Post‑marketing | Are adverse events being captured promptly? | Implement real‑world evidence studies; report to FAERS. |
| Access & pricing | Is the drug affordable for low‑income patients? | Offer tiered pricing; collaborate with insurers. |
| Off‑label use | Is there robust evidence before promotion? | Restrict marketing to approved indications. |
| Long‑term stewardship | How will we ensure ongoing safety monitoring? | Commit to PhaseIV trials and public data sharing. |
Following this checklist helps clinicians, regulators, and pharma teams keep patient welfare at the heart of every decision.
Conclusion
Aciderm illustrates how a promising drug can quickly become an ethical flashpoint. By scrutinizing safety data, guaranteeing genuine informed consent, tackling cost barriers, and demanding transparent marketing, we can turn that flashpoint into a steady, responsible light. The real test will be whether the entire health ecosystem-manufacturers, regulators, providers, and patients-chooses to act on these principles.
Frequently Asked Questions
Is Aciderm safe for people with liver disease?
Current trial data show a small increase in liver enzymes, but patients with pre‑existing liver conditions were largely excluded. Doctors should order baseline liver function tests and monitor them regularly if they prescribe Aciderm to this group.
What does ‘accelerated approval’ mean for Aciderm?
Accelerated approval allows the FDA to approve a drug based on surrogate endpoints, such as reduced gastric acidity, rather than definitive clinical outcomes. The trade‑off is that the sponsor must conduct post‑marketing studies to confirm real‑world benefit.
Can I get Aciderm if I don’t have insurance?
GastroPharm offers a patient‑assistance program that covers up to 80% of the cost for qualifying low‑income patients. Eligibility requires proof of income and a prescription from a licensed provider.
Are there any off‑label uses that are supported by evidence?
So far, evidence for off‑label use in functional dyspepsia comes from small case series, not randomized trials. Until larger studies confirm benefit, clinicians should prescribe Aciderm only for its approved indication.
How will adverse events be reported after Aciderm is on the market?
Healthcare providers must submit reports to the FDA’s FAERS system. GastroPharm also runs a voluntary registry that collects patient‑reported outcomes for ongoing safety evaluation.
kevin joyce
August 31, 2025
Aciderm arrives at a crossroads where pharmacological innovation meets the perennial moral dialectic that has haunted biomedicine since its inception. The ontological weight of a novel acid‑secreting pathway forces us to interrogate the epistemic foundations of surrogate endpoints versus hard clinical outcomes. In the realm of beneficence, the 42% symptom reduction is tantalizing, yet the trio of hepatic enzyme spikes casts a shadow on the principle of non‑maleficence. Autonomy becomes a fragile construct when consent forms gloss over uncertainties, thereby subordinating patient agency to the imperatives of market expediency. The justice axiom is imperiled by a $250 monthly price tag that stratifies access along socioeconomic lines, reinforcing health inequities. Moreover, the accelerated approval framework, predicated on surrogate biomarkers, transfers the burden of proof to the post‑marketing surveillance infrastructure, a domain too often under‑resourced. One must also contemplate the ethical ramifications of off‑label enthusiasm that outpaces evidentiary support, a phenomenon that erodes trust and inflates healthcare costs. The post‑marketing Phase IV studies, if robustly designed, could serve as a corrective feedback loop, yet the current one‑year horizon appears insufficient to capture chronic sequelae. Transparency of raw trial data would empower independent meta‑analyses, a requisite for the pluralistic vetting of safety signals. In the absence of such openness, the scientific community is relegated to a curated narrative that may understate risk. The ethical checklist delineated herein offers a pragmatic scaffold, but its efficacy hinges upon collective adherence by regulators, clinicians, and pharmaceutical stakeholders alike. Ultimately, the moral calculus surrounding Aciderm is not a static equation but a dynamic tableau requiring perpetual recalibration as real‑world evidence accrues. Only through vigilant stewardship can the promise of this therapeutic advance be reconciled with the imperatives of human dignity and equitable care.
michael henrique
September 6, 2025
Aciderm’s pricing strategy is an outright assault on American patients. A $250 monthly supply is downright obscene when generic PPIs cost a fraction of that. The market thinks it can get away with premium pricing for incremental benefit, but that’s a reckless gamble on public health.
Jamie Balish
September 12, 2025
Hey folks, let’s remember that any new drug brings both hope and responsibility. The therapeutic gains of Aciderm are exciting, yet we must champion robust post‑marketing studies to truly understand long‑term safety. Engaging patients in shared decision‑making can bridge the gap between efficacy data and real‑world concerns. By fostering open dialogue, clinicians empower individuals to weigh benefits against unknowns. Together, we can ensure that innovation serves everyone, not just a privileged few.
michael abrefa busia
September 17, 2025
Great points on patient empowerment 😊. It’s crucial that doctors don’t just hand out prescriptions without a full conversation. Supporting patients with clear info can really make a difference.
Dorothy Anne
September 23, 2025
Price transparency is essential.
Brufsky Oxford
September 29, 2025
Aciderm’s accelerated approval raises red flags; we need concrete outcome data. 😕 The surrogate metrics are not enough to guarantee real benefit.
Lisa Friedman
October 5, 2025
i think the articel is missing the part about the long term liver effects. its crazy how they dont mention that in the main body. people woud love to see a deeper dive.
cris wasala
October 11, 2025
agree with lisa but the article kinda covers the basics anyway
Tyler Johnson
October 16, 2025
From a broader perspective, the ethical landscape surrounding Aciderm is a microcosm of modern pharmacotherapy. While the therapeutic promise is undeniable, the accelerated pathway circumvents the traditional rigor that safeguards patient welfare. This tension underscores the necessity for a balanced approach that honors innovation while preserving the core bioethical tenets of beneficence, autonomy, and justice. Only through vigilant oversight and transparent communication can we navigate these murky waters without compromising the trust that is foundational to the patient‑physician relationship.
Annie Thompson
October 22, 2025
Reading through the whole piece, I’m struck by how the narrative weaves together scientific detail with ethical nuance. The author does a solid job of highlighting the tension between accelerated approval and the moral duty to ensure long‑term safety. However, the discussion could benefit from a deeper exploration of how socioeconomic disparities intersect with drug pricing, especially given the high cost of Aciderm. It’s also worth noting that while the checklist is helpful, its practical implementation will require coordinated effort across multiple stakeholders. Overall, the article is a thoughtful contribution that invites further dialogue on how we can responsibly integrate breakthrough therapies into patient care.
Parth Gohil
October 28, 2025
Totally agree! The ethical checklist is spot‑on, but we need real‑world data to back it up. In my experience, post‑marketing registries can surface rare adverse events that trials miss. Let’s push for more robust data sharing.
VAISHAKH Chandran
November 3, 2025
Data sharing is a noble ideal but the pharma lobby will inevitably obstruct it minimalist approach is required to cut through the noise
Pat Merrill
November 9, 2025
Oh great, another “miracle drug” with a price tag that screams, “We’re richer than you.” Thanks for the checklist, but the real solution is a price drop, not more paperwork.
Vicki Roth
November 14, 2025
I’m curious how the long‑term nutrient absorption impact will be studied. The article mentions it but doesn’t detail the methodology.
Vishal Bhosale
November 20, 2025
Honestly the methodology sounds like a mess. They’ll just sprinkle some surveys and call it a study.
Garima Gauttam
November 26, 2025
Well, if they’re going to do “surveys” why not just ask patients if they like the taste? That’s the real metric.
Georgia Nightingale
December 2, 2025
The drama of a drug that promises relief yet carries hidden risks is the stuff of modern medical theater. While the author’s checklist attempts to bring order, the real story is about power dynamics between big pharma and the everyday patient. Will we see a standing ovation for safety, or will the curtain fall on a costly experiment?
Viji Sulochana
December 8, 2025
Sounds like we need more open data and cheaper prices. Let’s keep the conversation going and make sure everyone gets a fair shot at treatment.